India Ups the Game on Cancer Care and Urban Health
India’s latest national workshop on cancer care and urban health delivered one message: move care closer to citizens and tighten systems. With DCCCs, new guidelines and a revamped NUHM framework, the country is gearing up for a real shift in public health delivery.


New Delhi [India], November 29: India just delivered a fantastic sight: policymakers, cancer specialists, state leaders and public health veterans sitting under one roof, speaking one language — urgency. And honestly, it’s about time.
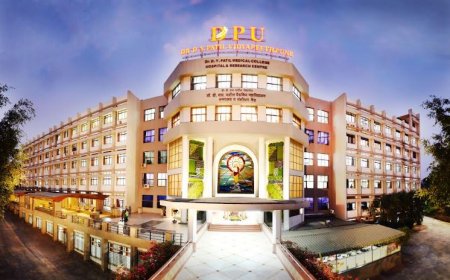
India’s fight against non-communicable diseases, especially cancer, is entering a sharper, more disciplined phase. At the two-day National Workshop on strengthening cancer care and urban health, held on 27–28 November at Sushma Swaraj Bhawan, the Union Health Ministry sketched a confident roadmap. The theme was clear early on — cancer care and urban health aren’t parallel lanes anymore; they’re converging into a single, integrated system.
Cancer care and urban health anchored almost every major discussion, beginning with the inaugural address from Union Health Secretary Punya Salila Srivastava. She cut straight to the point: cancer services must move closer to people, not the other way around.
Building District-Level Cancer Capacity
The centrepiece of the new push is the rollout of Day Care Cancer Centres (DCCCs) across every district. Announced in the Union Budget 2025–26, these centres are expected to decentralise chemotherapy, follow-up care and standardised treatment. For millions who currently travel to overcrowded tertiary hospitals, this shift could be the difference between delayed care and early survival.
Look, Indians are used to taking three buses and a train to get a basic scan. But that’s not how a confident, growing nation should operate. DCCCs aim to change that narrative with a district-first model.
Srivastava emphasised a seamless continuum of cancer care — from screening at community level to treatment at district facilities and advanced interventions when required. The backbone of this reform is the National Programme for Prevention and Control of NCDs (NP-NCD), now armed with revised training modules, freshly released at the workshop.
Policy Documents That Actually Matter
The Health Secretary also unveiled several key documents that will influence service quality nationwide:
- NP-NCD Training Modules
- FRU Guidelines 2025
- Operational Guidelines for Strengthening Laboratory Services under the Free Diagnostics Initiative
These aren’t decorative PDFs. They’re supposed to become everyday playbooks for health teams in districts, labs, and front-line facilities.
Participants dug into presentations on DCCC models, cancer workflows, digital dashboards, viral hepatitis screening integration, and quality assurance mechanisms under NQAS. If implemented right, this could be a strong pivot toward evidence-driven cancer management.
States Show Their Cards
Public health often looks top-down, but in practice, states run the show. Odisha, Tamil Nadu and Madhya Pradesh came ready — showcasing everything from community-led cancer screening drives to robust district-level oncology pathways. Their models proved one thing: scalable solutions don’t need to be fancy; they need to be consistent.
Experts from NHSRC, Tata Memorial Centre, AHPGIC Odisha, NCDC and ICMR threw in deep technical insight. The national panel’s deliberations circled around predictable but crucial themes: early detection, multidisciplinary care, referral efficiency and district-level capacity-building.
States reaffirmed rollout of DCCCs, adoption of uniform treatment workflows and strengthening of referrals from Ayushman Arogya Mandirs. If you’ve ever watched cricket in a small town, you know that local champions — not top stars — keep the game alive. District health teams will play that role here.
Urban Health Takes the Spotlight
Day two shifted from cancer to cities. With urbanisation sprinting ahead, India’s urban health challenge is no longer a side issue — it’s the main event.
Srivastava reminded states and UTs that urban health requires constant adaptation. The National Urban Health Mission (NUHM) is being retooled to match the speed and complexity of today’s cities.
Additional Secretary & Mission Director (NHM) Aradhana Pattnaik pushed for city-specific strategies rather than cut-copy-paste models. Joint Secretary (Policy) Saurabh Jain walked participants through the revised NUHM framework aimed at strengthening service delivery in towns and metros.
Discussions leaned heavily on infrastructure, service efficiency, referral pathways and tighter convergence between Urban Local Bodies and state governments. Simply put, the country wants urban primary healthcare that actually works — not clinics that exist only on paper.
States shared innovations in urban clinics, mobile medical units, digital tracking, and community-driven models. As India’s cities swell, learning from each other isn’t optional anymore — it’s survival strategy.
The Road Ahead
The Ministry’s closing note was blunt: urban primary healthcare must become more accessible, equitable and resilient, especially for the poorest urban families — the daily-wage workers, migrants, and informal sector warriors who keep Indian cities running.
Cancer care and urban health now sit at the center of India’s public health priorities. The reforms announced at the workshop are ambitious, but with political backing, state ownership and technical clarity, they could reshape how healthcare reaches ordinary Indians.
And if you’ve ever had chai outside a district hospital, you know people aren’t asking for miracles. They just want timely treatment, clear pathways and dignity in care. This workshop set the stage. Implementation will decide the scorecard.
Also Read: Constitution Day India: PM’s Powerful Call to Duty and Democratic Pride
What's Your Reaction?